
Outpatient Evaluation
Radiation oncologists collect the patient's medical history and conduct necessary examinations to
assess whether proton radiotherapy is suitable for the patient. Based on the evaluation, treatment plan
will be determined.


Positioning and Immobilization
Once the treatment plan is confirmed, technicians will create personalized immobilization devices (such
as thermoplastic masks or vacuum bags) tailored to the patient’s treatment area. These devices ensure
high reproducibility of the patient’s position during treatment, which is essential for precise radiotherapy

Simulation and Image Fusion
After immobilization, the patient undergoes a CT scan (CT-sim) to obtain dedicated DICOM images. If
necessary, an MRI scan (MRI-sim) may also be performed. Preoperative/postoperative or pre-chemotherapy/
post-chemotherapy MRI, CT, or PET images are imported into the system and fused with the
CT-sim images to accurately contour the tumor location and extent. This step is critical for optimizing
treatment planning and ensuring precise radiotherapy delivery.

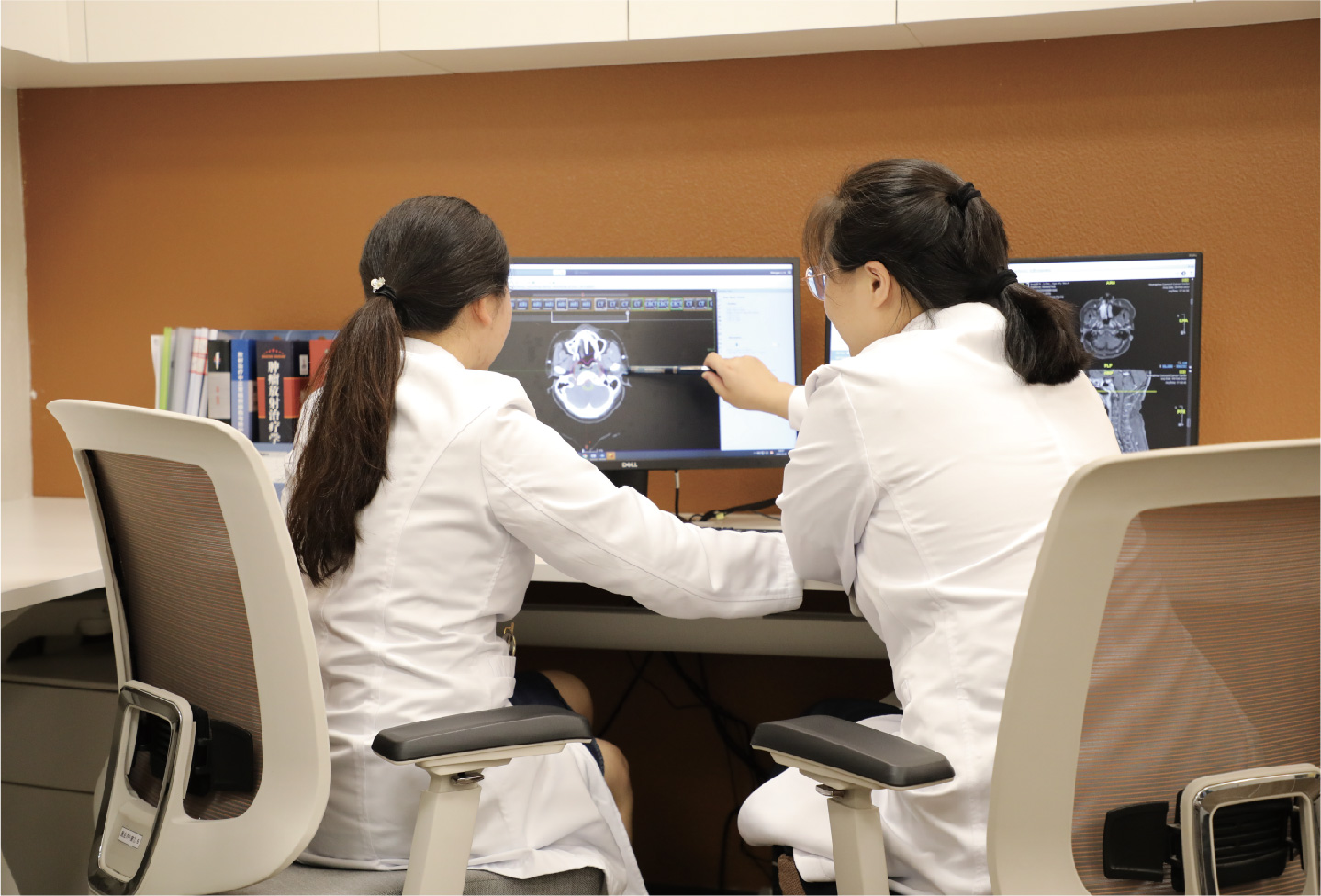
Target Delineation and Dose Prescription
Using the CT-sim and fused images, radiation oncologists delineate the precise boundaries of the tumor
and identify normal tissues that need protection. They then prescribe the appropriate radiation dose and
fractionation for the tumor target area while setting tolerance doses for surrounding healthy tissues.


Proton Treatment Plan Formulation
Based on the prescribed dose and target volume, medical physicists use the treatment planning system to
design the number and direction of radiation fields. Through iterative optimization, they achieve the best
possible dose distribution and treatment plan. Radiation oncologists evaluate the plan to ensure it meets the
dose requirements for both the target area and normal tissues with the best dose optimization.


Proton Treatment Plan Verification
The proton radiotherapy plan is verified under simulated treatment conditions to ensure its safety, accuracy
and feasibility. The plan is only approved for actual treatment after successful verification.


Proton Radiotherapy Delivery
Technicians position the patient according to the immobilization conditions and take verification images.
After confirming precise positioning through image guidance, the treatment is delivered based on the
treatment plan. Each fraction generally lasts 20–30 minutes.


Follow-Up Visits During Proton Therapy
Patients see physicians weekly during radiotherapy. Radiation oncologists actively monitor and manage acute side effects, track tumor regression, and adjust the treatment plan as needed.


Post-Proton Radiotherapy Follow-Up
The follow-up schedule is determined by the patient’s specific condition and disease type. Generally,
patients are advised to attend follow-up visits every 3 months for the first 1–2 years after treatment, every 6
months for year 3–5, and annually thereafter. Tumor control will be evaluated and any long-term side effects
will be monitored, recorded and managed.

